Medical updates: The majority of cervical cancer cases (99%) are associated with high-risk human papillomavirus (HPV) infection. HPV is a very prevalent virus that is spread through sexual contact. Although the majority of HPV infections are self-limiting and symptomless, persistent infections can lead to cervical cancer in females.
In the Eastern Mediterranean region, cervical cancer is the sixth most frequent malignancy in women. In the Region, an estimated 89 800 women are expected to receive a cervical cancer diagnosis in 2020, and more than 47 500 women will pass away from the illness.
January is Cervical Cancer Awareness Month.
It is the ideal chance for WHO and its collaborators to increase public awareness of cervical cancer and HPV vaccination. The topic of Cervical Cancer Awareness Month this year is the eradication of cervical cancer.
Also read : https://medicalupdates.in/2022/11/28/cancer-causing-chemicals-found-in-sanitary-napkins/
As long as it is identified early and carefully handled, cervical cancer is one of the most successfully treatable types of cancer when it is diagnosed. With the right medical care and palliative care, cancers that have already advanced to advanced stages can also be controlled. Within a generation, cervical cancer as an issue for public health can be solved with a comprehensive strategy for prevention, screening, and treatment.
What is Cervical Cancer?
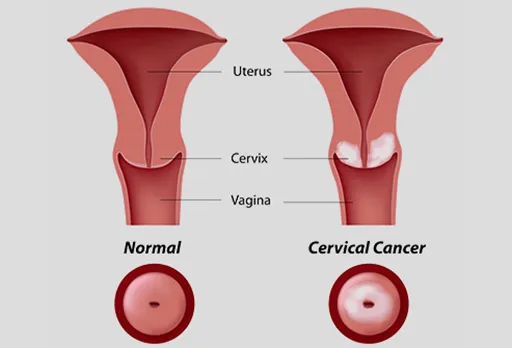
The cells lining the cervix, or lower portion of the uterus, are where cervical cancer first develops (womb). The uterus’s body, which is where a fetus develops, is joined to the vagina by the cervix (birth canal). Cancer develops when the body’s cells start to proliferate out of control.
The cervix is divided into two sections and has two different types of cells covering it.
- The opening of the cervix that enters the uterus is known as the endocervix. There are glandular cells all throughout it.
- During a speculum exam, the doctor can see the exocervix (also known as the ectocervix), that is the exterior portion of the cervix. It has squamous cells all over it.
The transformation zone is the region in the cervix where these two cell types merge. With age and pregnancy, the precise location of the transformation zone shifts. The cells in the transformation zone are where the majority of cervical malignancies start.
Causes, Risk Factors, and Prevention

HPV infection causes cervical cancer
Virtually all cervical cancers are brought on by long-lasting (persistent) infection with high-risk varieties of human papillomavirus (HPV).
At some point in their lives, almost everyone who engages in sexual activity will contract the HPV virus. HPV infections with a high-risk (cancer-causing) HPV type account for almost half of all cases. Along with cervical cancer, high-risk HPV can also lead to a number of other cancers. The high-risk strains of HPV that lead to the majority of cervical cancer occurrences include HPV16 and HPV18.
As the immune system manages the infection, the majority of HPV infections disappear on their own. Long-term high-risk HPV infections can alter the cervical cells in ways that, if left untreated, can develop into cancer.
Your risk of cervical cancer may also be increased by other factors like:
Having a weakened immune system: The body’s capacity to combat HPV infection and other illnesses may be diminished as a result. Immunocompromised individuals are more prone than non-immunocompromised individuals to experience chronic HPV infections and develop into cancer. Immunocompromised individuals include those who:
- Have HIV infection or another disease that affects immunity.
- Take medication to reduce your immune response, for example, to treat cancer, treat autoimmune diseases, or to prevent organ rejection after a transplant.
Smoking or breathing in secondhand smoke: Cervical cancer is more likely to occur in people who smoke or breathe in secondhand smoke. The risk rises with daily cigarette consumption and duration of smoking.
Becoming sexually active at an early age: People who start having sexual relations before the age of 18 and those who have had several sexual partners are at a higher risk of developing a high-risk HPV infection that is persistent and ultimately results in cervical cancer. The likelihood of being exposed to high-risk HPV is increased by this sexual history.
Other reproductive factors: Cervical cancer risk has been linked to both the use of oral contraceptives (birth control pills) and having several children. These associations’ causes are not completely clear.
Also read: https://medicalupdates.in/2022/11/05/obesity-drug-helps-teens-lose-weight-study-finds/
DES exposure is a rare cause of cervical cancer
An independent risk factor for clear cell adenocarcinoma, a kind of cervical cancer, is exposure to the medication diethylstilbestrol (DES) during pregnancy. Some pregnant women in the United States received DES between 1940 and 1971 in order to avoid miscarriage (the premature birth of a foetus that cannot survive) and early labour. Clear cell adenocarcinoma of the vagina and cervix, as well as cervical cell abnormalities, are more common in women whose mothers used DES while they were expecting.
Cervical cancer is preventable
If detected early, cervical cancer is extremely treatable and highly preventive. By receiving an HPV vaccine, having regular cervical cancer screenings, and receiving the proper follow-up care when necessary, nearly all cervical malignancies might be avoided.
HPV vaccination
Cervical cancer can be prevented safely and effectively with the HPV vaccine. The FDA has authorised the Gardasil 9 vaccine for use in American females and males aged 9 to 45. All seven of the cancer-causing HPV strains that Gardasil 9 targets—16, 18, 31, 33, 45, 52, and 58—are prevented in approximately 100% of cases. It also stops the majority of genital warts.
Timing of HPV vaccination
Given that HPV is sexually transmitted, the HPV vaccine is most effective when administered prior to an individual beginning sexual activity. The vaccine may be less effective for people who are already sexually active. This is because some of the HPV strains the vaccine is designed to prevent may have been exposed to sexually active individuals.
The series can begin as early as age 9, but the Centers for Disease Control and Prevention advises routine HPV immunization for girls and boys at age 11 or 12. HPV vaccine is advised for young person’s up to the age of 26 who did not receive it within the recommended age range. Some adults between the ages of 27 and 45 who have not yet received the HPV vaccine may elect to do so.
Cervical cancer screening
Cervical cancer screening with HPV and Pap testing is also an important approach to prevent the disease. These tests can detect precancerous conditions that can be treated before they progress to cancer, including abnormal cell alterations. As a result, starting in their early 20s, it is crucial for women who have a cervix to have frequent screening exams.
Because HPV vaccination doesn’t protect against all HPV types that can cause cervical cancer, it’s still important to get screened at regular intervals.