“A scientific story of stealth assassin, the cancer causing bacteria H.pylori”

What is Helicobacter pylori?
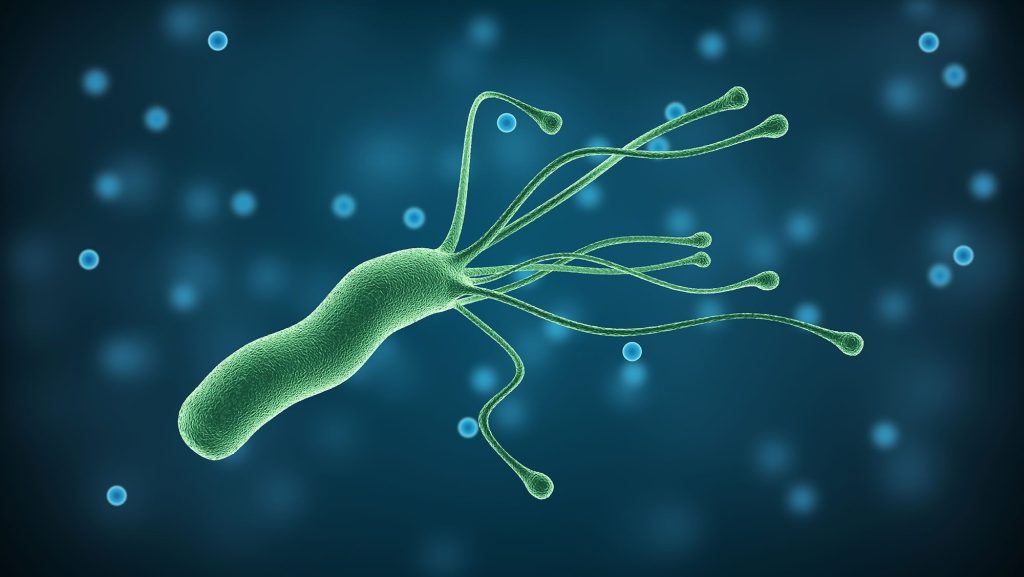
Helicobacter pylori (H. pylori) is a gram-negative, spiral shaped microaerophilic bacterium that was discovered by Marshall and Warren to infect the epithelium of the stomach. It has been found to have infected roughly half of the world’s population, making it one of the most common human infectious agents worldwide which belongs to the phylum Proteobacteria, class Epsilonproteobacteria, order Campylobacterales, family Helicobacteraceae, genus Helicobacter.
Is it a Carcinogen?
In 1994, H. pylori were classified as a class I biological carcinogen by the World Health Organization’s International Agency for Research on Cancer. In 2015, the Kyoto Global Consensus Report on Helicobacter pylori identified H. pylori as an infectious disease. In 2021, the National Toxicology Program’s 15th Report on Carcinogens added chronic infection with H. pylori to its list of substances that are known or reasonably anticipated to cause cancer in humans. In 2022, the United States Department of Health and Human Services listed H. pylori as a definite carcinogen.
How it survives in acid environment?
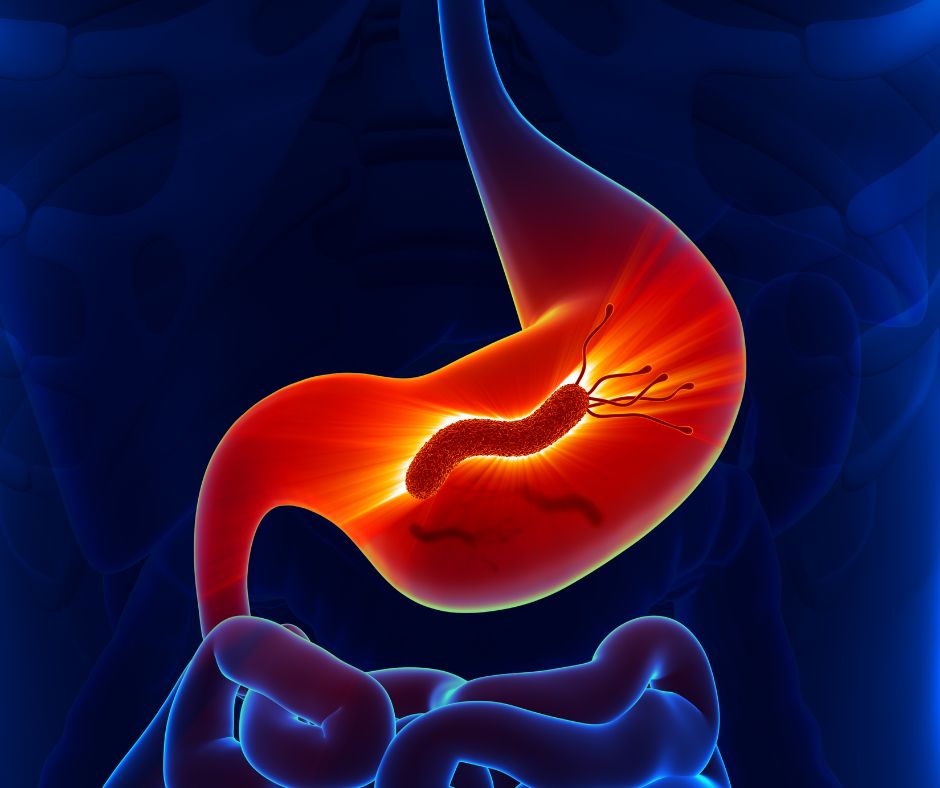
While other microorganisms and viruses are unable to survive in the harsh acidic conditions (pH < 2) of the stomach, H. pylori colonizes the stomach by penetrating the gastric mucous layer to reach the epithelial cell layer (pH 5–6). Additionally, H. pylori can neutralize surrounding acid through the secretion of urease, an enzyme responsible for converting urea into bicarbonate and ammonia. In this newly acquired niche, H. pylori continues to thrive as a monoculture and continuously elicits the host’s cellular and humoral immune responses to the site of infection. Consequently, the death of immune and epithelial cells at the site of the immune response provides nutrients to the gastric pathogen, allowing for continued colonization of the stomach over the lifespan of the host.
How does it get transmitted?
The H. pylori infection is transmitted from person to person through oral contact with stool (fecal–oral), saliva (oral–oral), or vomit (gastric–oral). In most populations, the bacterium is first acquired during childhood. Infection is more likely in children living in poverty, in crowded conditions, and in areas with poor sanitation.
Contaminated Food or Water: Ingesting food or water contaminated with H. pylori is a significant transmission route, particularly in areas with poor sanitation.
Fecal-Oral Route: In areas with inadequate sanitation, the bacteria can spread from fecal matter to the mouth via contaminated hands or surfaces.
Person-to-Person Contact: Close contact with an infected person, including sharing utensils or cups, can facilitate transmission.
There is limited evidence to suggest that Helicobacter pylori (H. pylori) can be transmitted through breast milk. Some studies have detected H. pylori DNA in breast milk, but the bacteria’s viability and the risk of transmission through this route are not well established
H.pylori transmission through kissing?
Yes. Helicobacter pylori (H. pylori) can be transmitted through kissing.
Saliva: H. pylori has been found in the saliva of infected individuals, making it possible for the bacteria to be transmitted through saliva exchange during kissing.
Oral Hygiene: Poor oral hygiene and dental plaque can harbor H. pylori, increasing the risk of transmission through close contact such as kissing.
Close Contact: Family members or people living in close quarters are more likely to share H. pylori due to the higher likelihood of saliva contact and shared eating utensils.
While kissing is a potential route of transmission, it’s not the most common way the bacteria spreads.
Nobel prize story: The discovery of H.pylori
Barry J. Marshall and Robin Warren, two Australian researchers who discovered the bacterium Helicobacter pylori and deciphered its role in gastritis and peptic ulcer disease, have been awarded this year’s Nobel Prize in Physiology or Medicine. The Nobel Assembly at the Karolinska Institute has honored them for their unexpected but paradigm shift discovery that revealed that gastritis, and ulceration of the stomach or duodenum, were the result of infection with some curved Gram negative bacilli.
At that time when Warren and Marshall announced their findings, it was a long-standing belief in medical teaching and practice that stress and lifestyle factors were the major causes of peptic ulcer disease. Warren and Marshall rebutted that dogma, and it was soon clear that H. pylori, causes more than 90% of duodenal ulcers and up to 80% of gastric ulcers. The clinical community, however, met their findings, with skepticism and a lot of criticism and that’s why it took quite a remarkable length of time for their discovery to become widely accepted. They had to just push it harder and harder with all experimental and clinical evidences. In 1985, for example, Marshall underwent gastric biopsy to put evidence that he didn’t carry the bacterium, then deliberately infected himself to show that it in fact caused acute gastric illness. This ‘self-help’ experiment was published in the Medical Journal of Australia to describe development of a mild illness over a course of 2 weeks, which included histologically proven gastritis. This extraordinary act of Marshall demonstrated extreme dedication and commitment to his research that generated one of the most radical and important impacts on the last 50 year’s perception of gastroduodenal pathology. Their research made H. pylori infection one of the best-studied paradigms of pathogen biology, paving way for intense and hectic basic and clinical research activity leading to about 25,000 scientific publications till date. To realize the tremendous response of scientific and clinical communities, a dedicated journal called ‘Helicobacter’ was also started.
Does H. pylori cause cancer or other diseases?
Yes. Although H. pylori infection does not itself cause illness, Chronic H. pylori infection causes peptic ulcers (ulcers of the stomach and upper small intestine) and long-lasting inflammation in the stomach (called non-atrophic gastritis) in most people.. This inflammation can lead to several possible conditions, including atrophic gastritis (thinning of the stomach lining caused by long-term inflammation) and certain types of stomach (gastric) cancer, particularly gastric adenocarcinoma and gastric mucosa-associated lymphoid tissue (MALT) lymphoma, which is a rare type of non-Hodgkin lymphoma.

Pathophysiology
H. pylori’s pathogenicity is attributed to several virulence factors, including urease, cytotoxin-associated gene A (CagA), and vacuolating cytotoxin A (VacA). These factors enable the bacterium to colonize the acidic environment of the stomach, evade the host immune response, and induce inflammation.
- Urease: This enzyme hydrolyzes urea to produce ammonia, neutralizing gastric acid and creating a more favorable environment for bacterial survival.
- CagA: The CagA protein, delivered into host cells via a type IV secretion system, disrupts cellular signaling pathways, leading to increased inflammation and cellular proliferation.
- VacA: This toxin induces vacuole formation in gastric epithelial cells, contributing to cell damage and apoptosis.
The chronic inflammation induced by H. pylori can lead to mucosal damage, peptic ulcers, and, over time, precancerous changes such as atrophic gastritis and intestinal metaplasia. Persistent infection and inflammation create a microenvironment conducive to genetic mutations and cancer development.
Clinical Manifestations
The clinical outcomes of H. pylori infection range from asymptomatic gastritis to severe gastrointestinal diseases:
- Peptic Ulcer Disease (PUD): H. pylori is a leading cause of peptic ulcers, affecting the stomach and duodenum. Symptoms include epigastric pain, nausea, and bloating.
- Gastric Cancer: Chronic H. pylori infection is a significant risk factor for gastric adenocarcinoma, accounting for a substantial proportion of cases worldwide. Symptoms of gastric cancer are often nonspecific and may include weight loss, anorexia, and persistent abdominal pain.
- Mucosa-associated Lymphoid Tissue (MALT) Lymphoma: H. pylori infection can lead to the development of MALT lymphoma, a type of cancer affecting the stomach’s lymphoid tissue.
What factors increase the likelihood that H. pylori infections will be harmful?
Several factors affect the likelihood that an infection with H. pylori will cause cancer. Some of these factors are features of the bacterium itself. For example, some strains of H. pylori make a toxin called CagA that gets injected into the junctions where cells of the stomach lining meet. Once inside cells, CagA can cause them to become cancerous by removing controls on cell growth and enhancing cell motility. Long-term exposure of cells to the toxin causes chronic inflammation. Epidemiology studies suggest that CagA-positive strains have a stronger association with non-cardia gastric cancer than CagA-negative strains .
Some evidence also suggests that certain lifestyle exposures may modify H. pylori–induced stomach cancer risk. For example, H. pylori–infected individuals who smoke have a higher risk of stomach cancer than H. pylori–infected individuals who do not smoke. Also, a high intake of salt and processed meat is associated with an increased risk of stomach cancer, possibly by increasing the risk that H. pylori will colonize the stomach or that CagA will enter gastric cells.
Diagnosis
The diagnosis of H. pylori infection can be achieved through various methods:
- Non-invasive Tests:
- Urea Breath Test: Measures the presence of urease activity.
- Stool Antigen Test: Detects H. pylori antigens in feces.
- PCR:A lab test called a stool polymerase chain reaction (PCR) test can detect H. pylori infection in stool. The test can also identify mutations that may be resistant to antibiotics used to treat H. pylori .
- Serology: Identifies antibodies against H. pylori, though it cannot distinguish between active and past infections.
- Invasive Tests:
- Endoscopy with Biopsy: Allows for direct visualization and histological examination of the gastric mucosa. Biopsies can be subjected to rapid urease testing, culture, and histopathology.
Treatment
Standard treatment is bismuth quadruple therapy: proton pump inhibitor (PPI) or H2-blocker + bismuth + metronidazole + tetracycline. Clarithromycin triple therapy (PPI + clarithromycin + amoxicillin or metronidazole) is an option in regions where H. pylori clarithromycin resistance is known to be <15% and in patients with no previous history of macrolide exposure.
Recently, combination therapies using rifabutin have become available, especially for refractory cases. Longer treatment durations (14 days vs. 7 days) provide higher eradication success rates.
Prevention
Based on the results of recent studies, the following measure may help to reduce transmission of H. pylori bacteria:
- Practice good hygiene and hand washing, especially with food preparation.
- All patients with chronic gastrointestinal symptoms that may be associated with H. pylori infection should be tested and treated to prevent exposure to family members.
- Patients should complete the full course of therapy (antibiotics and acid blockers) to maximize the potential for a cure.
- Maintain proper nutrition to prevent iron deficiency anemia.
- Increase cruciferous vegetable intake (ie. cauliflower, cabbage, and broccoli)
SOURCE: CDC, FDA, WHO, Medical updates

Written By Dr. RAJESWARI V