Medical updates: One of the most intricate processes in the human body is wound healing. Multiple cell types with distinct roles during the phases of hemostasis, inflammation, growth, re-epithelialization, and remodeling must be coordinated in both space and time. Phenotypic and functional variability within a few of these cell types has been discovered because of the development of single-cell technologies. Additionally, there have been findings of uncommon skin stem cell subsets that are unipotent in a healthy condition but multiply after skin damage.
Understanding the functions of each of these cell types and how they interact is crucial to comprehending the mechanisms of normal wound closure. The recruitment and activation of cells are directly impacted by changes in the microenvironment, which include modifications to mechanical pressures, oxygen levels, chemokines, extracellular matrix, and growth factor production.
This results in conditions of poor wound healing. In order to create efficient therapeutic treatments for healing wounds, single cell technologies can be used to understand these cellular modifications in pathological states including chronic wounds and hypertrophic scarring.
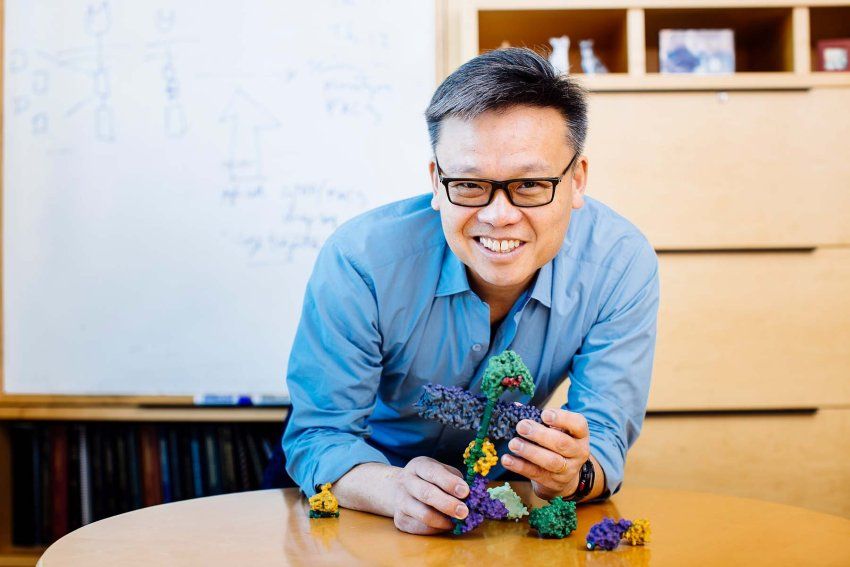
Researchers at UC San Francisco (UCSF) have engineered molecules that function as “cellular glue,” enabling them to precisely control how cells adhere to one another. The discovery is a significant step toward regenerative medicine’s long-term goal of creating new tissues and organs.
The body naturally contains adhesive molecules that hold the tens of trillions of cells together in intricate patterns. They build neural circuits, form structures, and direct immune cells toward their intended targets. In order to maintain the body’s ability to function as a self-regulating whole, adhesion also makes cell communication easier.
In a recent study, tailored adhesion molecules were designed into cells that joined with specified partner cells in predictable ways to build complex multicellular ensembles. The findings were published in the edition of Nature on December 12, 2022.
“We were able to engineer cells in a manner that allows us to control which cells they interact with, as well as the nature of that interaction,” said senior author Wendell Lim, PhD, the director of UCSF’s Cell Design Institute and the Byers Distinguished Professor of Cellular and Molecular Pharmacology. “This opens the door to building novel structures like tissues and organs.
Cell-Cell Regenerative Communication
Body organs and tissues start to grow in pregnancy and continue to do so throughout life. Many of the molecular instructions that control these generative processes by adulthood have disappeared, and some tissues, like nerves, are incapable of recovering from damage or illness.
By creating new connections between adult cells, Lim aims to overcome this. However, to achieve this, one must be able to precisely engineer how cells communicate with one another.
“The properties of a tissue, like your skin for example, are determined in large part by how the different cells are organized within it,” said Adam Stevens, PhD, the Hartz Fellow in the Cell Design Institute and the first author of the paper. “We’re devising ways to control this organization of cells, which is central to being able to synthesize tissues with the properties we want them to have.”
Also read: https://medicalupdates.in/2022/11/12/fda-alerts-health-care-professionals-of-risks-to-patients-exposed-to-xylazine-in-illicit-drugs/
The degree to which cells are linked together determines how distinct a tissue is. Many of the cells of a solid organ, such as the liver or lungs, will be very closely connected. The immune system, however, uses weaker connections to allow cells to go through blood vessels or squeeze between the tightly packed cells of skin or organ tissues in order to access a pathogen or a wound.
The researchers divided the design of their adhesion molecules into two portions to control that aspect of cell interaction. On the outside of the cell, a portion of the molecule functions as a receptor and determines which other cells it will interact with. The strength of the bond that formed is tuned by a second component located inside the cell. The two components are interchangeable in a modular method to produce a variety of specialized cells that bind in various ways across a range of cell types.
The Code Underlying Cellular Assembly
According to Stevens, these discoveries also have other uses. To make it simpler to investigate illness states in human tissue, researchers could, for instance, create tissues that imitate disease states.
Custom adhesion molecules may provide a fuller knowledge of how the transition from single to multicellular species began. Cell adhesion was a crucial milestone in the evolution of mammals and other multicellular organisms.
“It’s very exciting that we now understand much more about how evolution may have started building bodies,” he said.
“Our work reveals a flexible molecular adhesion code that determines which cells will interact, and in what way. Now that we are starting to understand it, we can harness this code to direct how cells assemble into tissues and organs. These tools could be really transformative.”